Blog
-
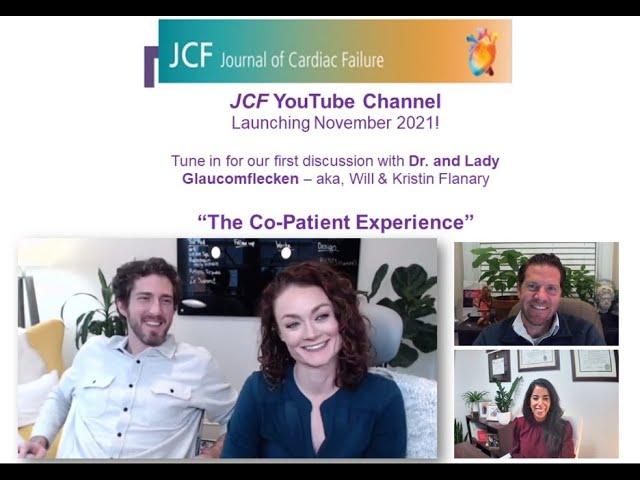
Dr. Will Flanary’s Sudden Cardiac Arrest Survival Story
Will Flanary, M.D., a young and healthy Ophthalmologist and Comedian (known as Dr. Glaucomflecken), suffered a Sudden Cardiac Arrest in his sleep. His wife, Kristin Flanary, saved his life by providing CPR. Will spoke to Avive about his experience, SCA
-
Critical Illness Cosurvivors: An Interview with Lady Glaucomflecken
“We all will be at the receiving end of critical illness for ourselves or our loved ones. It is almost guaranteed. A family’s needs are the blind spot of the overstretched and dysfunctional healthcare system that needs to be addressed.
-
Co-Survivors
“There are side effects to caregiving, and Kristin Flanary wants a health care system that recognizes the people who support patients when they leave doctors’ offices and hospitals. Before he had turned 35, Mrs. Flanary’s husband, Will Flanary, MD, had
-
Medscape: Dr. Glaucomflecken on Why We Can All Use a Laugh Right Now
Podcast interview by Dr. Eric Topol.
-
The Quiet Place
“One dark morning last May, I wrecked my body giving 10 minutes of CPR. My 34-year-old husband, Will, had been lying peacefully next to me, both of us fast asleep. I woke up suddenly to a loud noise I will